
Guilherme Movio
Background: Paediatric Tracheostomy is a procedure used to ventilate children through a hole in the trachea. Indications for the procedure were once primarily for acute upper airway obstruction, due to infections. Generally, there is poor knowledge surrounding tracheostomies with limited awareness of guidelines amongst health-care professionals.
Aim: To discuss the rationale for changes to the indications for tracheostomy in the paediatric population. I will also investigate the key complications related to the procedure and discuss the importance of awareness of an emergency algorithm for the multidisciplinary team.
Findings: Indications have changed due to advancements in medicine which have increased the life expectancy and survival rates of children with often life-threatening congenital conditions. Tracheostomies can offer these children long term ventilatory support. Upper airway obstructions due to infections are less frequent indications due to long running and successful vaccination programs. Current complications of tracheostomy are due to acute obstruction and inadvertent decannulation. Intra-operative complications are infrequent, due to refinement of surgical technique.
Conclusion: Paediatric airway management is a rapidly evolving field because of continuous advancements in neonatal and intensive care medicine. The indications and complications have changed over the last four decades. A greater understanding of tracheostomy complications amongst health-care professionals is required for better management.

Guilherme Movio
What is a tracheostomy?
A tracheostomy is a procedure where a hole is made into the trachea through the front of the neck to allow a cannula to be passed for ventilation support. They are used in the acute and chronic setting. Particularly, they are used within intensive care during the weaning process of mechanical ventilation [1].
How is a paediatric tracheostomies performed?
Surgical tracheostomies are indicated over percutaneous tracheostomies in the paediatric population. The procedure involves palpation of the anatomical landmarks to locate the cricoid cartilage and sternal notch to allow a horizontal incision to be made between the two landmarks. The platysma is then exposed and resected. Strap muscles are divided to expose the thyroid isthmus. This may be divided to expose the tracheal rings. A vertical or horizontal incison may be used, between the second to fourth tracheal rings. Once the trachea has been incised, an obturator is used. This is then removed and the canulla inserted. Unlike adults, no cartilage rings are removed. Flexible bronchoscopy can be used to visualise the tip of the tracheostomy above the carina [2,3].
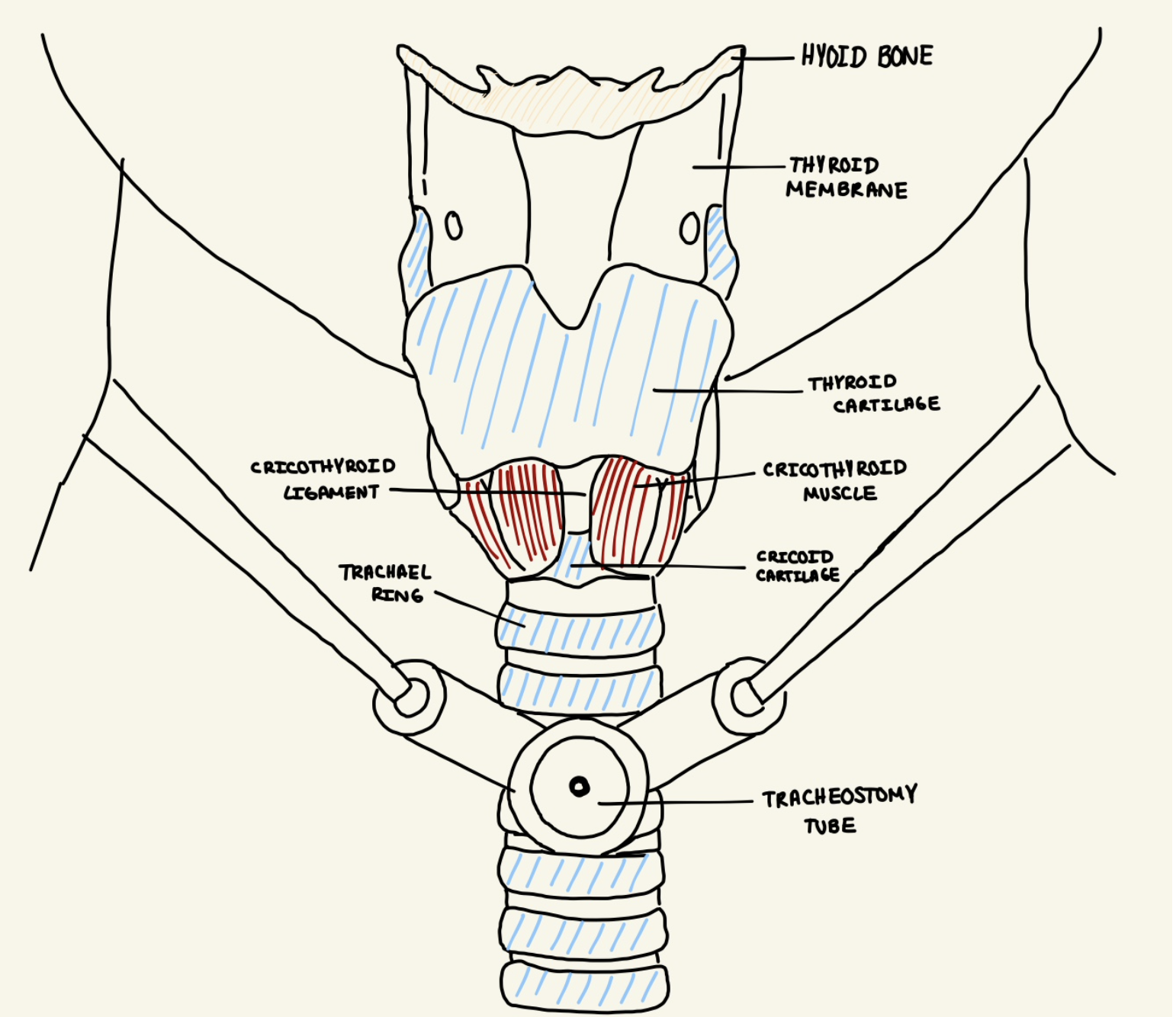
Figure 1. The airway anatomy with a tracheostomy in situ.
What are the differences between the adult airway and the paediatric airway?
Neonatal airways are significantly smaller than adults. The average diameter of the subglottis in a full-term baby is 3.5mm, increasing to 7mm in a teenager and then 10-14mm in a full grown adult [4].
Children have shorter and wider necks. The larynx is situated more anteriorly compared to adults. Palpation of the anatomical landmarks in children is harder due to the hyoid cartilage. Tracheal cartilages in infants are softer than adults, leaving them at greater risk of collapse. The mucosa of the subglottis and supraglottis are also more prone to oedema and inflammation [5].
How have the indications for tracheostomies changed?
Between 1960 and 1970, paediatric tracheostomies were indicated primarily as an emergency procedure for upper airway obstruction caused by infections such as epiglottitis, diphtheria and croup [6]. Vaccination programs against haemophilus influenzae and corynebacterium diphtheria have proved successful at reducing the incidences of these infections and consequently the cases of acute airway obstruction [7].
What are the complications of tracheostomies?
Tracheostomy related complications can be divided into intra-operative, early post-operative and late post-operative. This is highlighted in Table 1 [2].
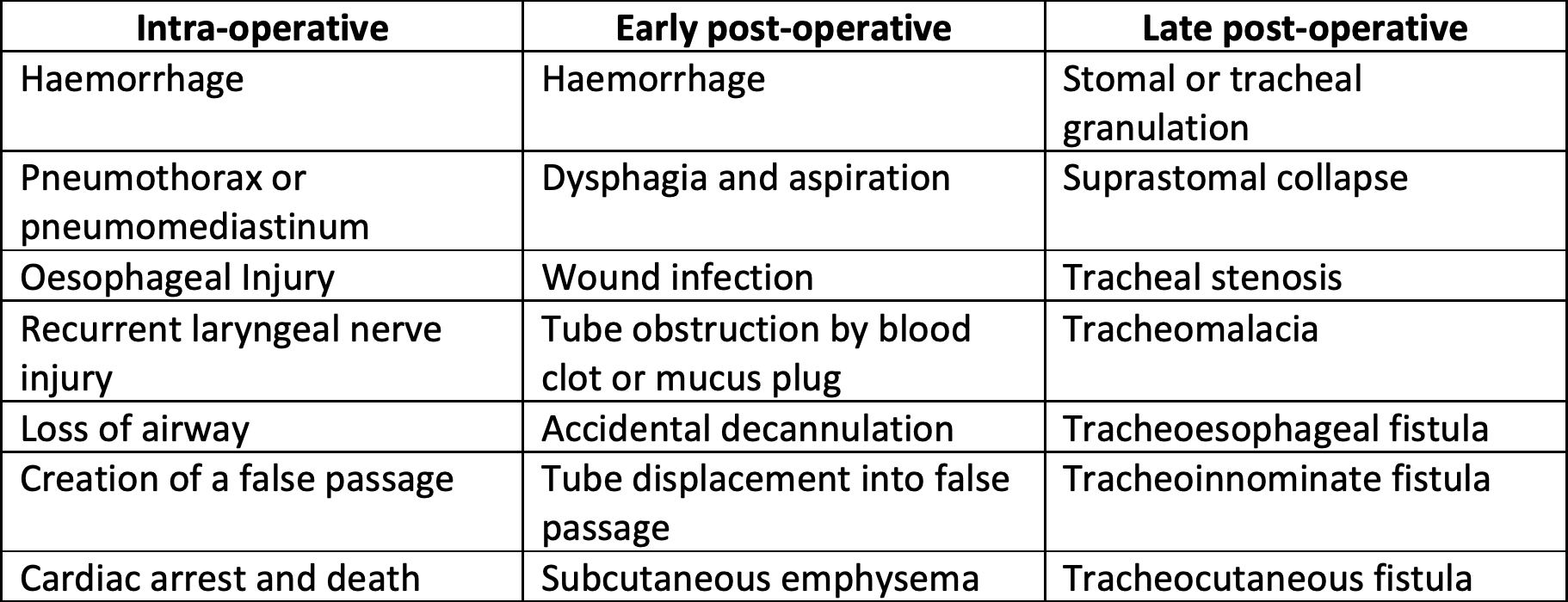
Table 1. Complications associated with tracheostomy.
What is the management of tracheostomies related acute complications in the post-operative setting?
A tracheostomy becomes the primary airway for a patient, delivering vital oxygen. Prompt management is therefore essential to prevent hypoxia. The National Audit Project 4 (NAP4) highlighted how 50% of airway related mortality and morbidity within intensive care were due to tracheostomy complications. The report also stated that up to 50% of intensive care trainees were not aware of the emergency algorithm. Figure 2 shows the algorithm [8].
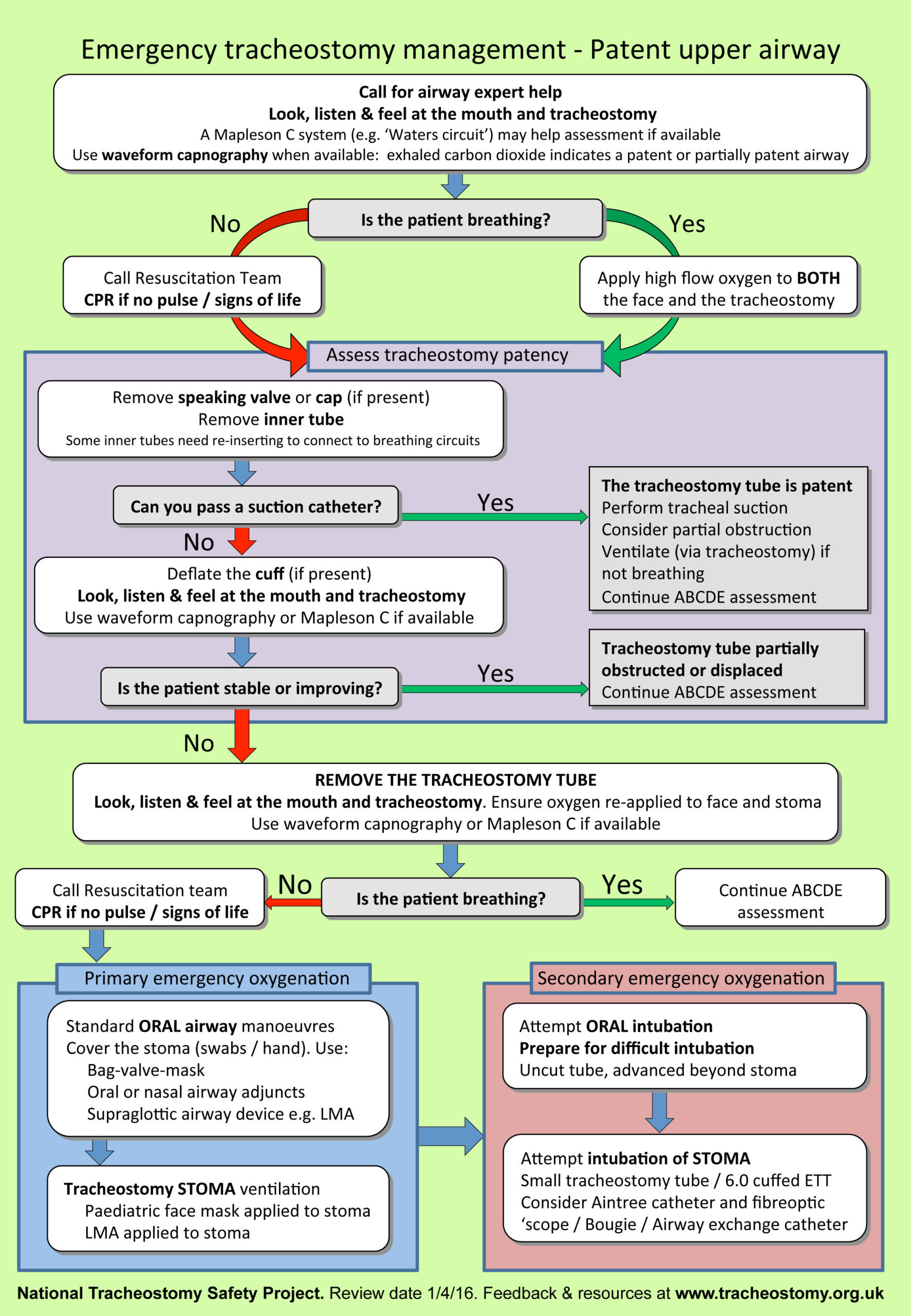
Figure 2. Emergency tracheostomy management algorithm.
Agknowledgements
I would like to thank Ms Shadaba Ahmed, Ears Nose and Throat Consultant at Royal Lancaster Infirmary for supporting me through my research project.
References:
1. Falimirski ME. Tracheostomy. Oper Tech Gen Surg. 2003;5(3):134–8.
2. Campisi P, Forte V. Pediatric tracheostomy. Semin Pediatr Surg. 2016;25(3):191–5
3. Engels PT, Bagshaw SM, Meier M, Brindley PG. Tracheostomy: from insertion to decannulation. Can J Surg. 2009 Oct;52(5):427–33.
4. Graham, J. (2008). Pediatric ENT. 1st ed. Berlin: Springer, p.183.
5.Watters KF. Tracheostomy in Infants and Children. Respir Care [Internet]. 2017 Jun 1;62(6):799 LP – 825.
6. Gill J, Bhardwaj B, Singla S. Changing trends in indications of pediatric tracheotomy: A tertiary care center experience. Journal of Laryngology and Voice. 2017;7(1):7-10.
7. Parrilla C, Scarano E, Guidi ML, Galli J, Paludetti G. Current trends in paediatric tracheostomies. Int J Pediatr Otorhinolaryngol. 2007;71(10):1563–7.
8. Doherty C, Neal R, English C, Cooke J, Atkinson D, Bates L, et al. Multidisciplinary guidelines for the management of paediatric tracheostomy emergencies. Anaesthesia. 2018;73(11):1400–17.
Slide 1 image (max 2mb)
Slide 1 video (YouTube/Vimeo embed code)
Image 1 Caption
Slide 2 image (max 2mb)
Slide 2 video (YouTube/Vimeo embed code)
Image 2 Caption
Slide 3 image (max 2mb)
Slide 3 video (YouTube/Vimeo embed code)
Image 3 Caption
Slide 4 image (max 2mb)
Slide 4 video (YouTube/Vimeo embed code)
Image 4 Caption
Slide 5 image (max 2mb)
Slide 5 video (YouTube/Vimeo embed code)
Image 5 Caption
Slide 6 image (max 2mb)
Slide 6 video (YouTube/Vimeo embed code)
Image 6 Caption
Slide 7 image (max 2mb)
Slide 7 video (YouTube/Vimeo embed code)
Image 7 Caption
Slide 8 image (max 2mb)
Slide 8 video (YouTube/Vimeo embed code)
Image 8 Caption
Slide 9 image (max 2mb)
Slide 9 video (YouTube/Vimeo embed code)
Image 9 Caption
Slide 10 image (max 2mb)
Slide 20 video (YouTube/Vimeo embed code)
Image 10 Caption
Caption font
Text
Image (max size: 2mb)
Or drag a symbol into the upload area
Image description/alt-tag
Image caption
Image link
Rollover Image (max size: 2mb)
Or drag a symbol into the upload area
Border colour
Rotate
Skew (x-axis)
Skew (y-axis)
Image (max size: 2mb)
Or drag a symbol into the upload area
Image description/alt-tag
Image caption
Image link
Rollover Image (max size: 2mb)
Or drag a symbol into the upload area
Border colour
Rotate
Skew (x-axis)
Skew (y-axis)
Image (max size: 2mb)
Or drag a symbol into the upload area
Image description/alt-tag
Image caption
Image link
Rollover Image (max size: 2mb)
Or drag a symbol into the upload area
Border colour
Rotate
Skew (x-axis)
Skew (y-axis)
Image (max size: 2mb)
Or drag a symbol into the upload area
Image description/alt-tag
Image caption
Image link
Rollover Image (max size: 2mb)
Or drag a symbol into the upload area
Border colour
Rotate
Skew (x-axis)
Skew (y-axis)